Causes of Lung Cancer in Non-Smokers: The Role of Asbestos and Other Key Factors
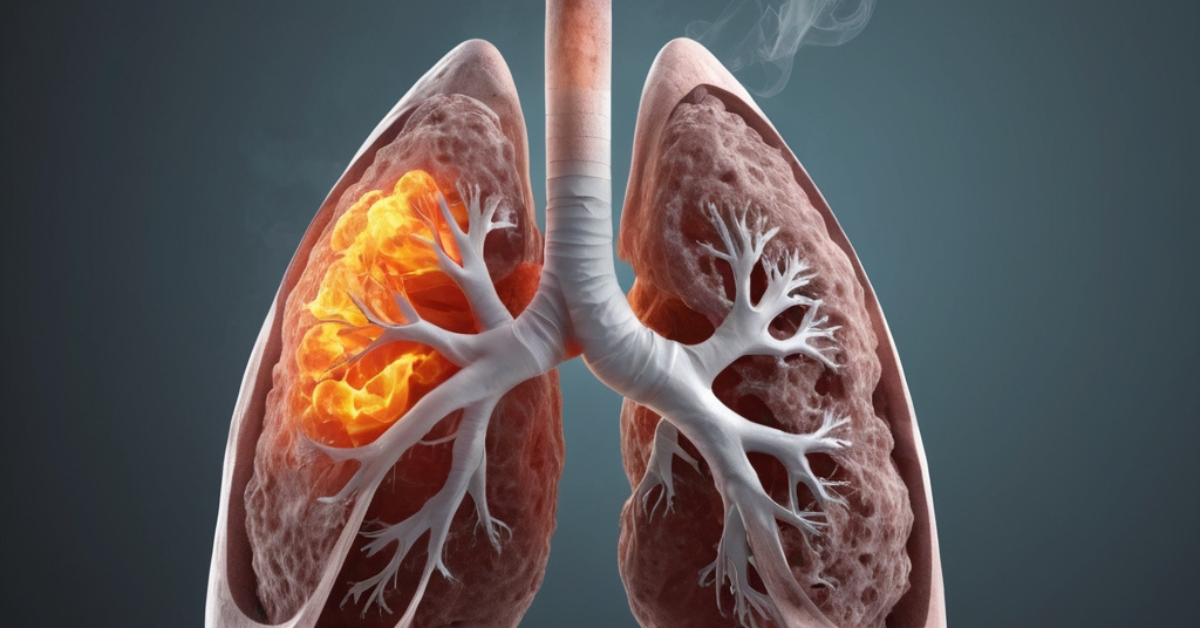
Lung cancer is widely linked to smoking, but non-smokers can also develop this serious condition due to various causes. Asbestos exposure is one of the most prominent factors, along with other environmental and genetic risks. This article explores the primary causes of lung cancer in non-smokers, with a particular focus on asbestos and how it contributes to lung cancer.
How Asbestos Exposure Impacts Non-Smokers
Asbestos is a naturally occurring mineral that has been used in various industries for its durability and resistance to heat. However, asbestos fibers are highly toxic when inhaled. When non-smokers are exposed to asbestos, even without a smoking history, they can still develop lung cancer. The fibers can embed themselves deep in lung tissue, leading to chronic inflammation, scarring, and ultimately cancerous cell growth.
Industries such as construction, shipbuilding, and automotive manufacturing have historically used asbestos in materials. Non-smokers who work in these environments face significant risks. The most concerning aspect is that lung cancer can develop decades after exposure, making asbestos a long-term health hazard. This highlights the importance of implementing strict safety measures in workplaces where asbestos is present.
Environmental Asbestos Exposure and Other Carcinogens
Non-smokers can also be exposed to harmful minerals in their everyday environment. In older homes and buildings, these minerals were often used for insulation, roofing, and fireproofing. Over time, these materials deteriorate, releasing dangerous fibers into the air. Non-smokers may unknowingly inhale these fibers, increasing their risk of developing lung cancer.
In addition to toxic minerals, other environmental carcinogens like radon gas, air pollution, and secondhand smoke contribute to lung cancer in non-smokers. Radon, a radioactive gas that can seep into homes through soil, is a major cause of lung cancer after smoking. However, harmful fibers remain one of the most potent carcinogens that non-smokers can encounter, often without their knowledge.
Environmental exposure to hazardous fibers is particularly dangerous for those living near industrial zones or contaminated sites. Unlike smoking, which is a personal choice, exposure to these toxic materials is often unavoidable. This emphasizes the need for stricter regulations to monitor and remove these fibers from homes, schools, and workplaces.
Occupational Risks of Asbestos Exposure
Certain occupations present a higher risk of exposure to dangerous fibers, even for non-smokers. Jobs in construction, shipbuilding, plumbing, and automotive repair commonly involve contact with materials containing these hazardous fibers. Workers tasked with demolition, renovation, or maintenance in older buildings are at particular risk of disturbing these fibers.
Although safety protocols have improved in recent decades, many older buildings and industrial sites still contain hazardous materials. Workers in high-risk jobs should be properly equipped with protective gear, and employers must follow strict removal procedures to prevent exposure. Non-smokers in these occupations remain vulnerable to lung cancer, and continuous monitoring of fiber levels is crucial to their safety.
The Role of Genetics in Asbestos-Related Lung Cancer
Genetics play a significant role in determining how susceptible a non-smoker might be to developing lung cancer after exposure to harmful fibers. Some people have genetic mutations that make their bodies more prone to cancer when exposed to carcinogens like these toxic materials. These genetic factors can amplify the effects of environmental exposure, leading to a higher likelihood of lung cancer in non-smokers.
For those with a family history of lung cancer or known genetic mutations, genetic testing can provide valuable insight into their risk levels. Understanding the interaction between genetics and exposure to hazardous fibers is important for physicians when developing personalized prevention and monitoring strategies for at-risk individuals.
Secondhand Smoke and the Risk of Asbestos Exposure
While toxic fibers are a primary concern, secondhand smoke further complicates the risk for non-smokers. Exposure to both hazardous fibers and secondhand smoke dramatically increases the likelihood of lung cancer. Non-smokers who live with smokers or work in environments where smoking occurs are at heightened risk.
Secondhand smoke contains carcinogens that, when combined with exposure to harmful fibers, create a deadly synergy. Reducing exposure to both toxic fibers and secondhand smoke is essential for lowering cancer risks among non-smokers. However, even in the absence of secondhand smoke, hazardous fibers alone remain a significant enough threat to cause lung cancer in non-smokers.
Steps to Reduce Asbestos Exposure and Prevent Lung Cancer
Reducing lung cancer risks among non-smokers begins with minimizing exposure to asbestos. Homeowners and businesses should be aware of the dangers posed by asbestos in older buildings, especially when planning renovations. Regular inspections and testing for asbestos should be part of routine maintenance in such structures.
Workers in high-risk industries must be educated on proper safety measures, including the use of protective gear and the implementation of safe removal procedures for hazardous fibers. Regulatory agencies should enforce stricter policies for handling and disposal of these toxic materials to minimize exposure risks in workplaces.
Public awareness campaigns about the dangers of harmful fibers and the importance of early detection can also help reduce lung cancer rates among non-smokers. Early detection of lung cancer increases survival rates, and understanding the potential risks from toxic materials can lead to more proactive health measures.
Conclusion
Lung cancer in non-smokers has several causes, with exposure to harmful fibers being one of the most significant. Non-smokers face a variety of risks, from occupational hazards to environmental contamination. While secondhand smoke, radon gas, and genetic predispositions contribute to the disease, toxic materials remain a leading cause of lung cancer.
Prevention efforts should focus on reducing exposure to hazardous fibers in all settings, improving public awareness, and enforcing strict regulations on their handling. By addressing these factors, we can significantly reduce the occurrence of lung cancer in non-smokers and create safer environments for everyone.
